Another group or vendor provides the info on the next page. If you don’t want to leave our site, choose the “X” in the upper right corner to close this message. Or choose “Go on to next website” to move forward.

Incentives for high-quality care
You can earn incentives for providing high-quality, efficient care in all payment models and even share financial risk in some.
VBP has also become a point of focus for [insert state health agency]. [The department] is moving toward innovative approaches to care coordination, population health management and VBP.
We're used to a health care system that takes care of people after they're already sick. The aim of VBP is to:
- Improve the member's health care experience
- Improve the health of individuals and populations
- Reduce the costs of health care
- Increase provider satisfaction
To meet these goals, VBP moves beyond sick care and adopts a proactive, comprehensive and data-driven approach to keeping people healthy.
Value-based payment continuum
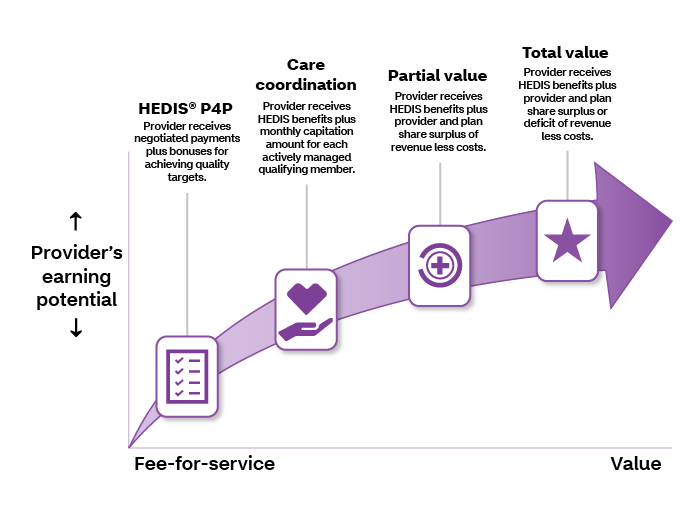
HEDIS® pay for performance (P4P)
HEDIS is the Healthcare Effectiveness Data and Information Set — standardized performance measures the National Committee for Quality Assurance (NCQA) developed for the managed care industry. You can use HEDIS data to ensure appropriate care for members by identifying and eliminating gaps in care.
You have the opportunity to take part in our HEDIS P4P program. The program pays you annual bonuses based on the measures you complete. Each measure has a specific incentive amount paid after you achieve a target score. P4P enhances quality of care by incentivizing you to focus on preventive and screening services.
Care coordination
To promote diligent and proactive engagement of members, we offer primary care physicians (PCPs) the opportunity to earn incentives. You can do so by committing to rigorous care coordination in partnership with our care management team.
When you take part, you’re eligible to receive a monthly capitation amount for each member assigned to you as their PCP. This is also known as per member per month (PMPM). It involves an active provider-patient or provider-client relationship. If you take part, you’ll have regularly scheduled meetings with our care management team to:
- Review selected member cases and progress
- Ensure active management of all members
You’ll have to meet program expectations to remain eligible for the PMPM fee.
Partial value
To further encourage preventive care, we give you the option to take part in partial-value shared savings agreements. A medical benefits ratio (MBR or medical loss ratio) is the sum of the assigned members’ medical expenses divided by the sum of their premium revenue. When you achieve this ratio goal we set, you’re paid part of the surplus related to their cost of care. These agreements incentivize you to actively engage members in preventive, low-cost outreach and care to prevent high-cost emergency department (ED) visits and inpatient admissions.
When you take part in a partial-value-based agreement, you’ll have more supports and resources, including robust and regular bi-directional data sharing with us. We expect you to progress to total-value-based agreements after one to two years.
Better health at lower costs: Why we need value-based care now (PDF)
Total value
The total-value program is the pinnacle of earning opportunities we offer. When you take part in total-value-based agreements, you have the opportunity to earn a greater part of surplus payments than those in partial-value-based agreements, while also being accountable for members’ costs.
Each year, providers in total-value-based agreements are paid part of the surplus or pay us part of the deficit related to their assigned members’ cost of care.
As with partial-value-based agreements, total-value-based agreements incentivize preventive, low-cost outreach and care to prevent high-cost, high-risk ED visits and inpatient admissions. With total-value-based agreements, you have access to advanced resources, data sharing and reporting.
Legal notices
HEDIS® is the property of the National Committee for Quality Assurance (NCQA).
